Want to save 25%? Check out our Subscriptions!
Rosacea is a chronic, inflammatory skin condition that primarily affects the face, leading to redness, pimples, swelling, and visible blood vessels. Often misunderstood and mistaken for other skin issues, Rosacea can be a source of discomfort and embarrassment for those affected.
Awareness and understanding are crucial in managing this condition effectively. This guide aims to provide a comprehensive look into Rosacea, from its history to modern-day management strategies, helping sufferers and the curious alike to learn about this common skin condition.
Rosacea is more than just a temporary blush. It is a persistent condition characterized by episodes of flare-ups and remissions. Despite being shared, it is often surrounded by misconceptions, leading to delayed diagnoses and treatment. Understanding Rosacea means recognizing its complexity and the need for personalized care approaches.
Rosacea’s history is as intriguing as the condition, showing how medical understanding and cultural perceptions of skin diseases have evolved over the centuries. The first person known to describe Rosacea medically was Dr. Guy de Chauliac, a French surgeon living in the 14th century. The term “Rosacea” itself comes from the Latin word “rosaceus,” meaning “rose-colored” or “rosy,” reflecting the characteristic redness associated with the condition. However, the journey to recognizing and categorizing Rosacea as a distinct medical condition is a fascinating narrative that spans several centuries and cultures.
Rosacea has likely afflicted humans for millennia, with descriptions that resemble the condition appearing in ancient medical texts. The earliest recorded accounts date back to the writings of physicians in ancient Rome, Greece, and Egypt, where it was often conflated with acne and other skin conditions due to the lack of a clear medical understanding of dermatological conditions. These early descriptions often attributed the redness and inflammation to excess blood or imbalances in bodily humor, a theory prevalent in medical thought until the late Renaissance.
During the Middle Ages, Rosacea was commonly referred to as “gutter rose” or “pustules of the face” in European medical literature. The condition was often treated with a mixture of herbal remedies, bloodletting, and dietary restrictions based on the prevailing medical theories of the time. It wasn’t until the 17th century that physicians began recognizing the condition as distinct from leprosy, which marked a significant advancement in dermatological diagnosis.
In recent decades, understanding the genetic components and immune responses associated with Rosacea and offering new avenues for treatment and management has become a significant concern.
The history of Rosacea is a testament to the progress of medical science and the evolving understanding of skin health. From its early conflations with other conditions to its recognition as a unique dermatological challenge, the journey of Rosacea through history reflects broader shifts in medical knowledge and societal attitudes towards skin conditions. Today, with ongoing research and an increasing number of treatment options, the future for those living with Rosacea is more hopeful than ever, offering the possibility of better management and an improved quality of life.
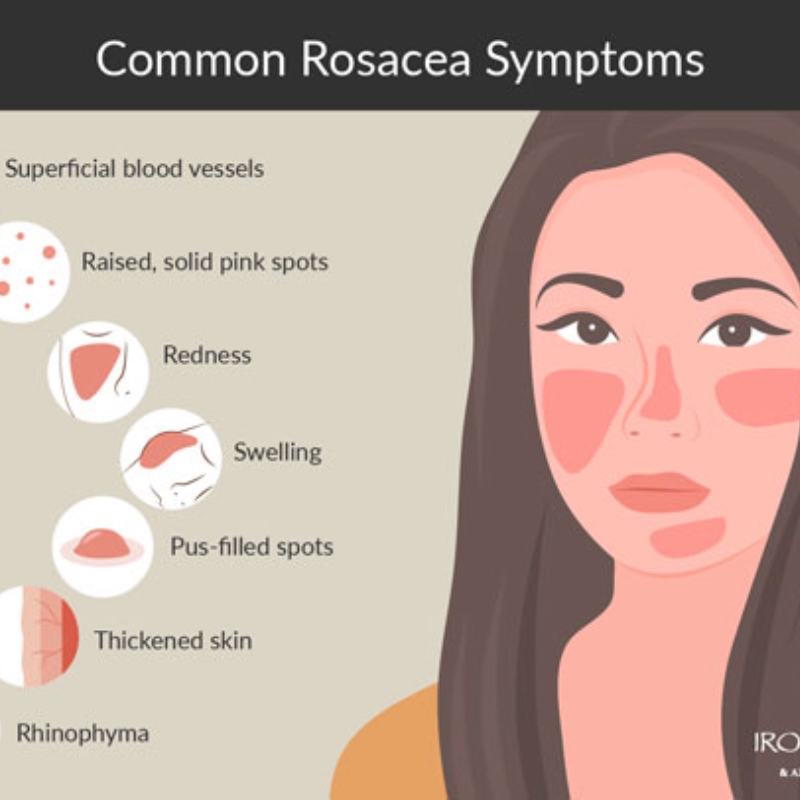
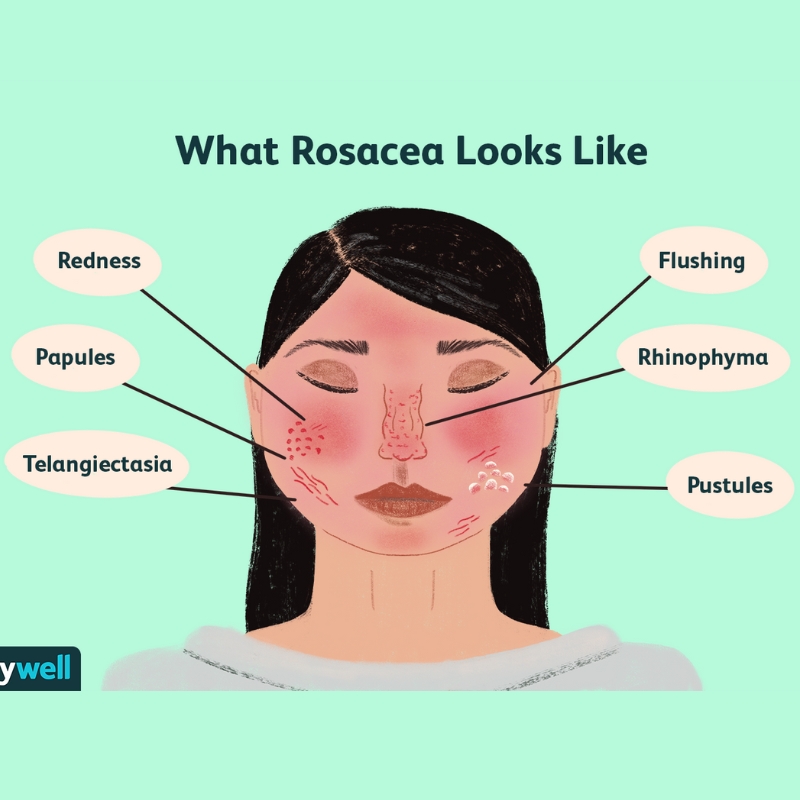
Rosacea’s symptoms vary widely among individuals but typically include facial redness, swollen red bumps, skin dryness, and eye irritation. These symptoms can fluctuate in severity and often escalate without proper management. Understanding the range of symptoms is vital for early recognition and treatment.
The exact cause of Rosacea remains unknown, but factors like genetics, vascular issues, skin peptides, and environmental factors are thought to play roles. Triggers such as stress, certain foods, alcohol, and weather changes can exacerbate symptoms, highlighting the importance of trigger identification and avoidance in management strategies.
Rosacea can significantly impact psychological and social well-being. The visible symptoms can lead to self-consciousness, anxiety, and social avoidance. Addressing the emotional and psychological aspects is as important as treating the physical symptoms, underscoring the need for a holistic approach to care.

Diagnosis typically involves a physical examination and a review of medical history. There’s no definitive test for Rosacea, making awareness of symptoms crucial for early detection and management. Dermatologists play a key role in diagnosing and guiding treatment plans.
Treatment for Rosacea may include topical medications, oral antibiotics, laser therapy, and lifestyle modifications. The goal is to control symptoms and prevent flare-ups. Treatment plans are often tailored to individual needs, reflecting the variable nature of the condition.
Living with Rosacea requires a comprehensive management strategy that includes medication, lifestyle adjustments, and skincare routines. Many succeed through trial and error, discovering what triggers to avoid and which treatments are most effective for their unique situation.
Preventive measures can help manage Rosacea effectively. These include protecting the skin from the sun, avoiding known triggers, and following a gentle skincare routine. Long-term management focuses on maintaining a balanced lifestyle and adhering to treatment plans.
Rosacea is a complex condition that requires a nuanced understanding and personalized approach to management. This guide aims to empower those affected with the knowledge and strategies needed for a better quality of life by demystifying its aspects- from history to treatment. Remember, Rosacea is manageable, and with the right approach, individuals can lead happy, fulfilling lives despite their condition.